6 Government-Sponsored Schemes For Cancer Patients In Karnataka
A cancer diagnosis can be a life-altering event that comes with a host of overwhelming emotional, mental, and financial challenges. Patients and their families struggle with feelings of uncertainty about treatment costs, which can be difficult to manage due to the complexity of medical bills and insurance coverage. In such times of medical crisis, the government has programs to help offset the cost of needed care.
Here are 5 government schemes offered by the state of Karnataka to provide treatment aid to cancer patients:
Here are 5 government schemes offered by the state of Karnataka to provide treatment aid to cancer patients:
Table of content:
1. Karnataka Chief Minister's Medical Relief Fund (KCMMRF)
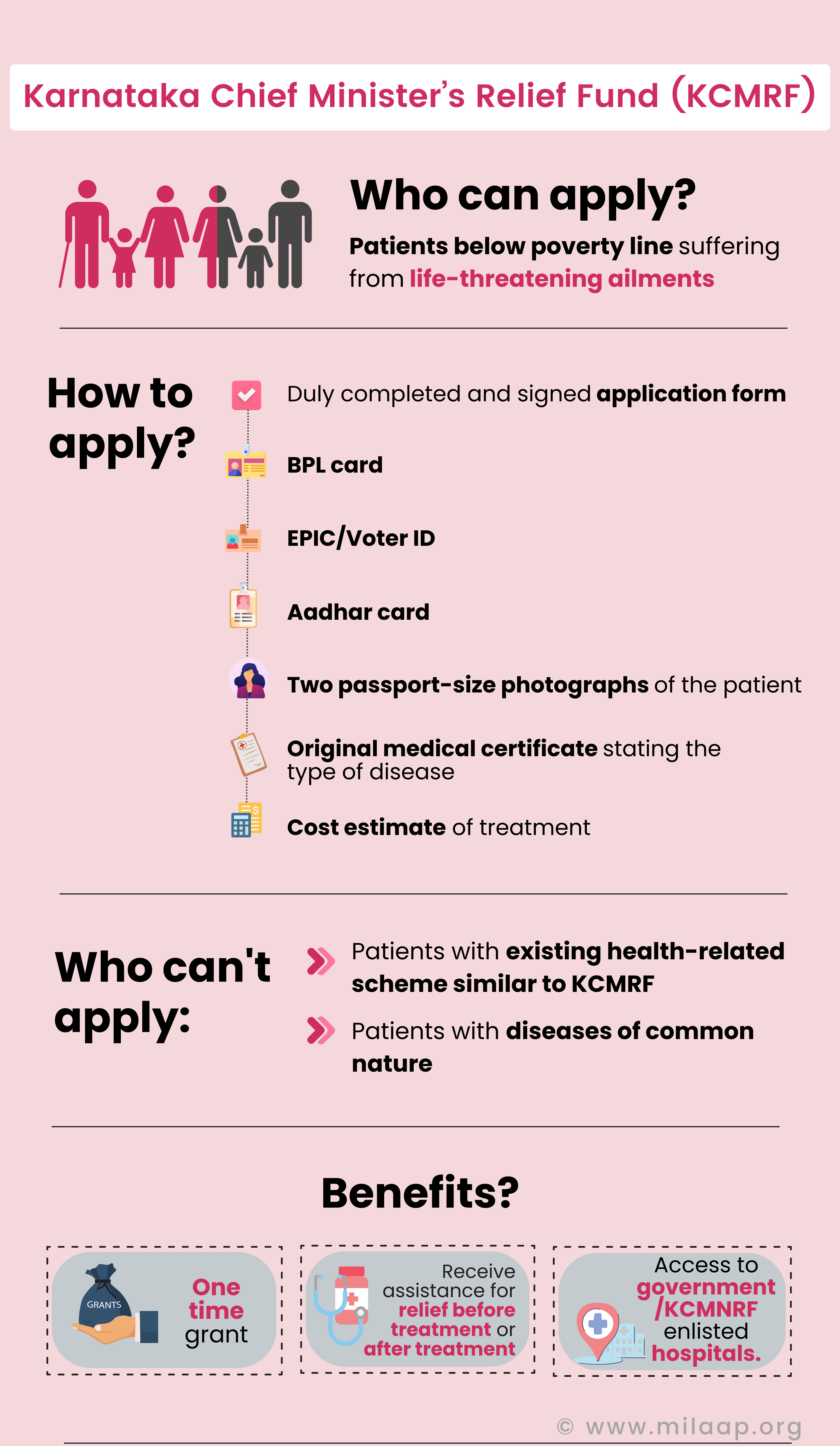
The KCMMRF grants financial assistance to patients below poverty line suffering from life-threatening ailments to receive treatment in any of the enlisted government hospitals, or non-enlisted hospitals of national repute in the state of Karnataka.
- KCMMRF runs on public contributions and does not receive any budgetary support.
- Patients are entitled to receive a maximum of ₹1 lakh for cancer treatment.
- Funds are allocated on the approval of the Chief Minister.
- A patient can apply for financial assistance for relief before treatment, or relief after treatment.
- To apply, the applicant will be required to produce a duly completed and signed application form, passport-size photo of patient, BPL card, EPIC and Aadhar card, original final hospital bill and discharge summary or estimation summary.
A patient is not eligible for financial assistance under KCMMRF, if:
- Their family is covered under Employees’ State Insurance Scheme (ESI), Central Government Health Scheme (CGHS) or any similar existing health-related scheme with provisions for reimbursements.
- The disease is of common nature with inexpensive treatments.
2. Ayushman Bharat - Arogya Karnataka Scheme (AB-ARK)
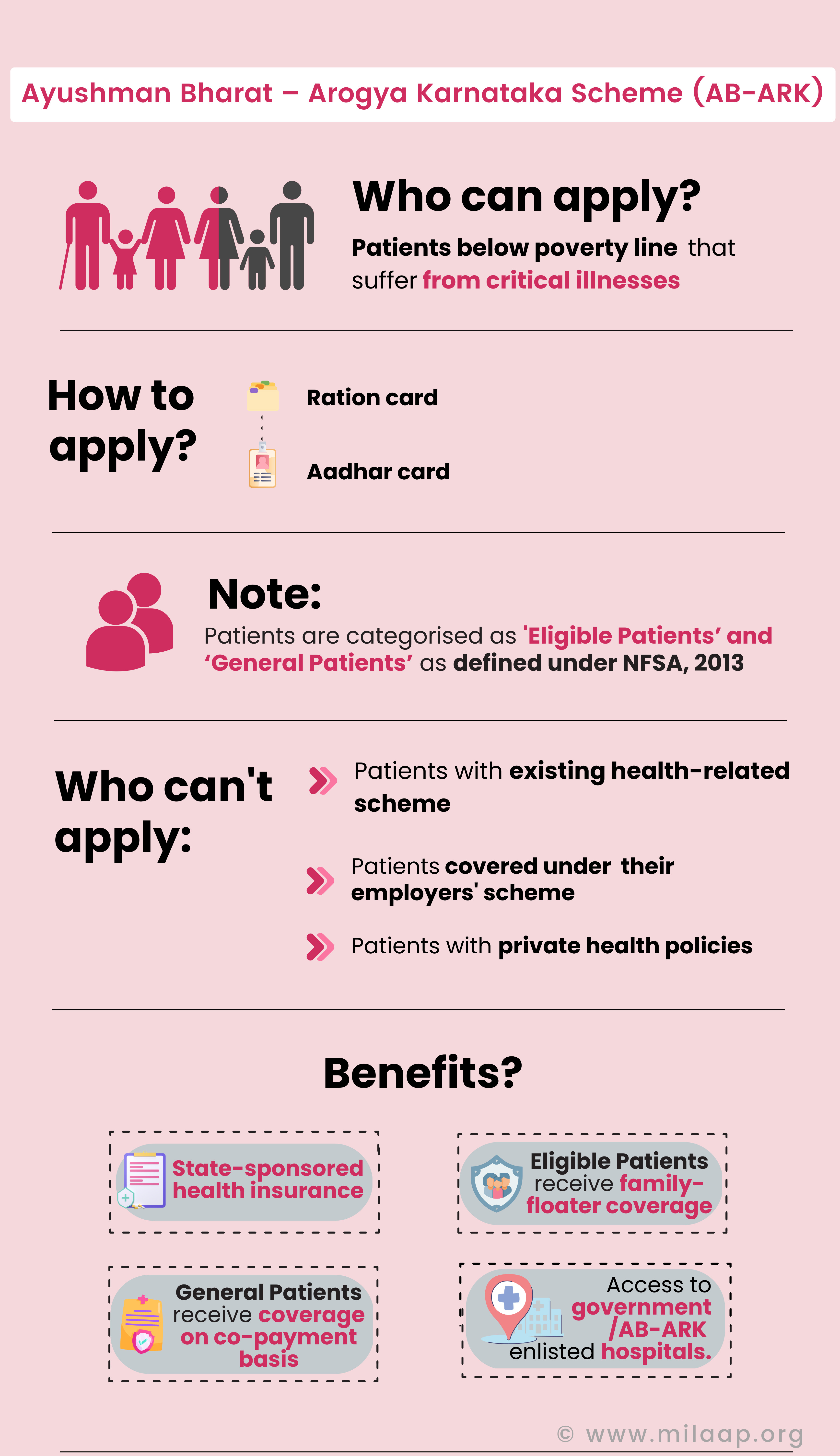
AB-ARK extends financial protection to patients living below poverty line that suffer from critical illnesses, to access primary, specified secondary and tertiary healthcare benefits at any of the enlisted hospitals within the state of Karnataka.
Read more about AB-ARK, here.
- Patients are classified as ‘Eligible Patients’ and ‘General Patients’ as defined under the National Food Security Act, 2013.
- Eligible Patients are entitled to receive family-floater coverage of up to ₹5 lakhs, per year for cancer treatment, while General Patients are entitled to receive coverage of up to ₹1.5 lakh per year, on a co-payment basis.
- To apply, the applicant will be required to produce their Aadhar card and ration card.
A patient is not eligible for financial assistance under AB-ARK, if:
- They are covered under Employees’ State Insurance Scheme (ESI) and Central Government Health Scheme (CGHS) .
- They are covered under the health insurance schemes of their employers.
- They have taken private health policies on their own.
Read more about AB-ARK, here.
3. Vajpayee Arogya Shree (VA)
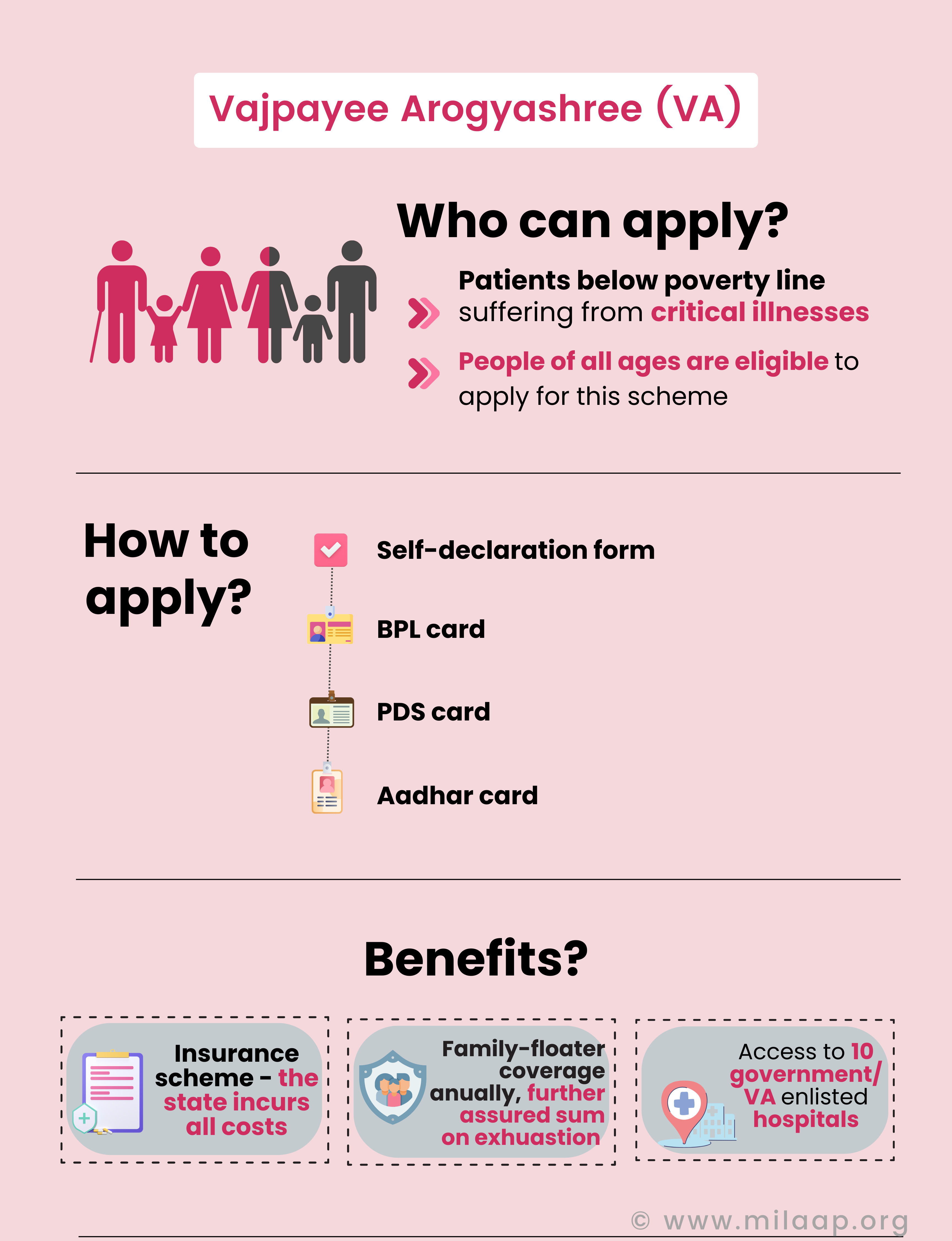
The VA insurance scheme was designed for patients below the poverty line suffering from critical illnesses, to increase their access to quality tertiary health care including hospitalisation, therapy and surgery.
Read more about VA, here.
- All costs are incurred by the state government.
- People of all ages are eligible to apply for this scheme.
- Provides family-floater coverage, i.e 5 members in a family can receive up to a sum of ₹1.5 lakh annually for cancer treatment, on exhaustion of which, a further ₹ 50,000 is provided.
- To apply, the applicant will be required to produce a self-declaration form, along with their Aadhar card, BPL card and PDS card.
Read more about VA, here.
4. Rajiv Arogya Bhagya (RAB)
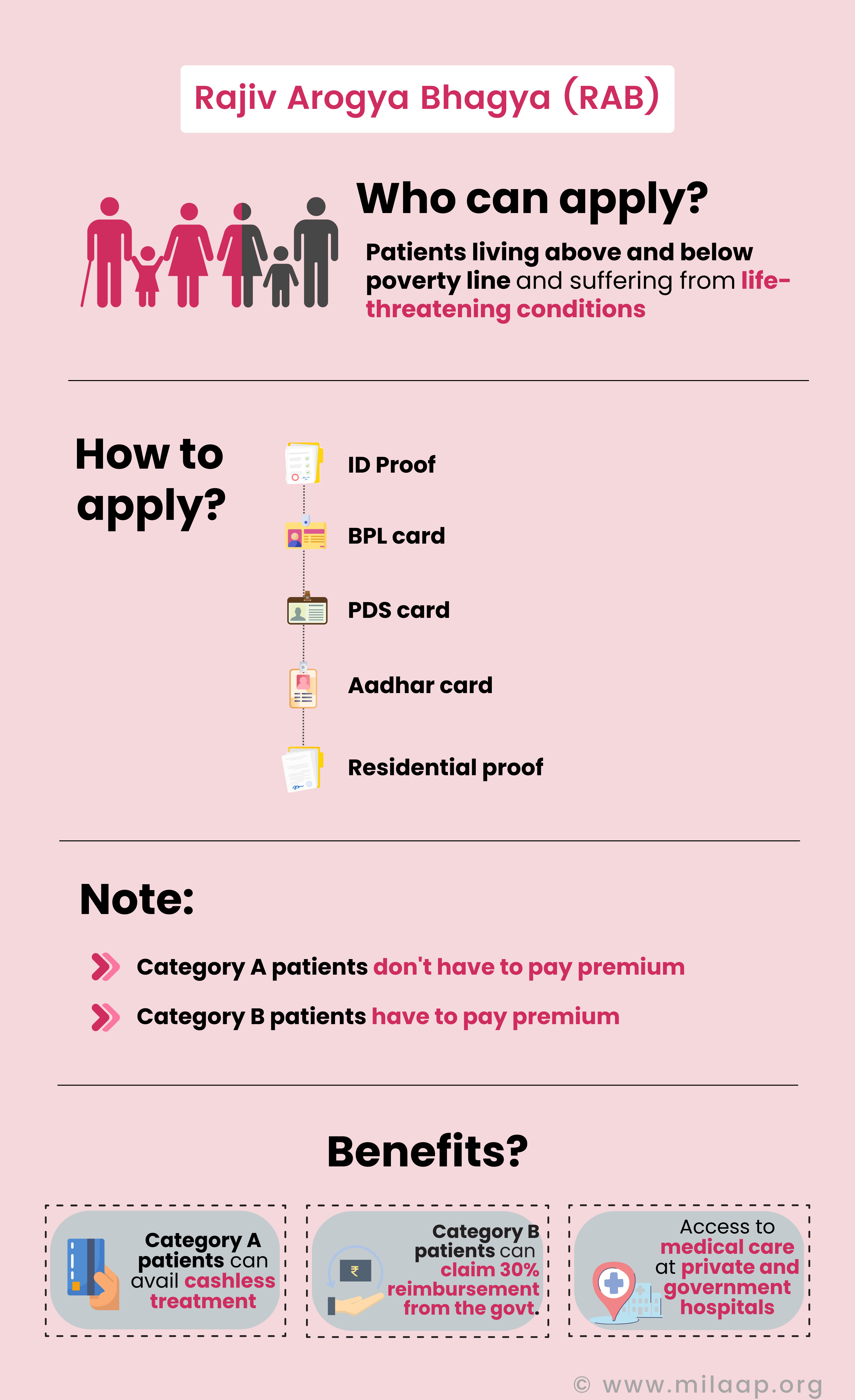
RAB is a state-sponsored health insurance scheme for patients living above poverty line and suffering from life-threatening conditions, to avail affordable and accessible tertiary treatment.
Read more about RAB, here.
- Patient must be a legal resident of the State of Karnataka.
- Patients can avail medical treatment at government and private hospitals.
- As there is no predetermined income bar, both APL and BPL patients can apply for this scheme.
- Patients who fall under Category A, i.e farmers labourers of unorganised sector, deprived households, SC/ST people, government employees, members of cooperatives societies, media persons and representatives, need not pay a premium.
- Whereas patients not included in Category A fall under Category B and have to pay a premium of ₹300, if hailing from rural areas, and ₹700 if failing from urban areas.
- Category A patients can avail cashless treatment, while Category B patients can claim 30% reimbursement from the government.
- To apply, the applicant will be required to produce ID proof, ration card, Aadhar card, PDS card and residential proof.
Read more about RAB, here.
5. Jyothi Sanjeevini Scheme (JSS)
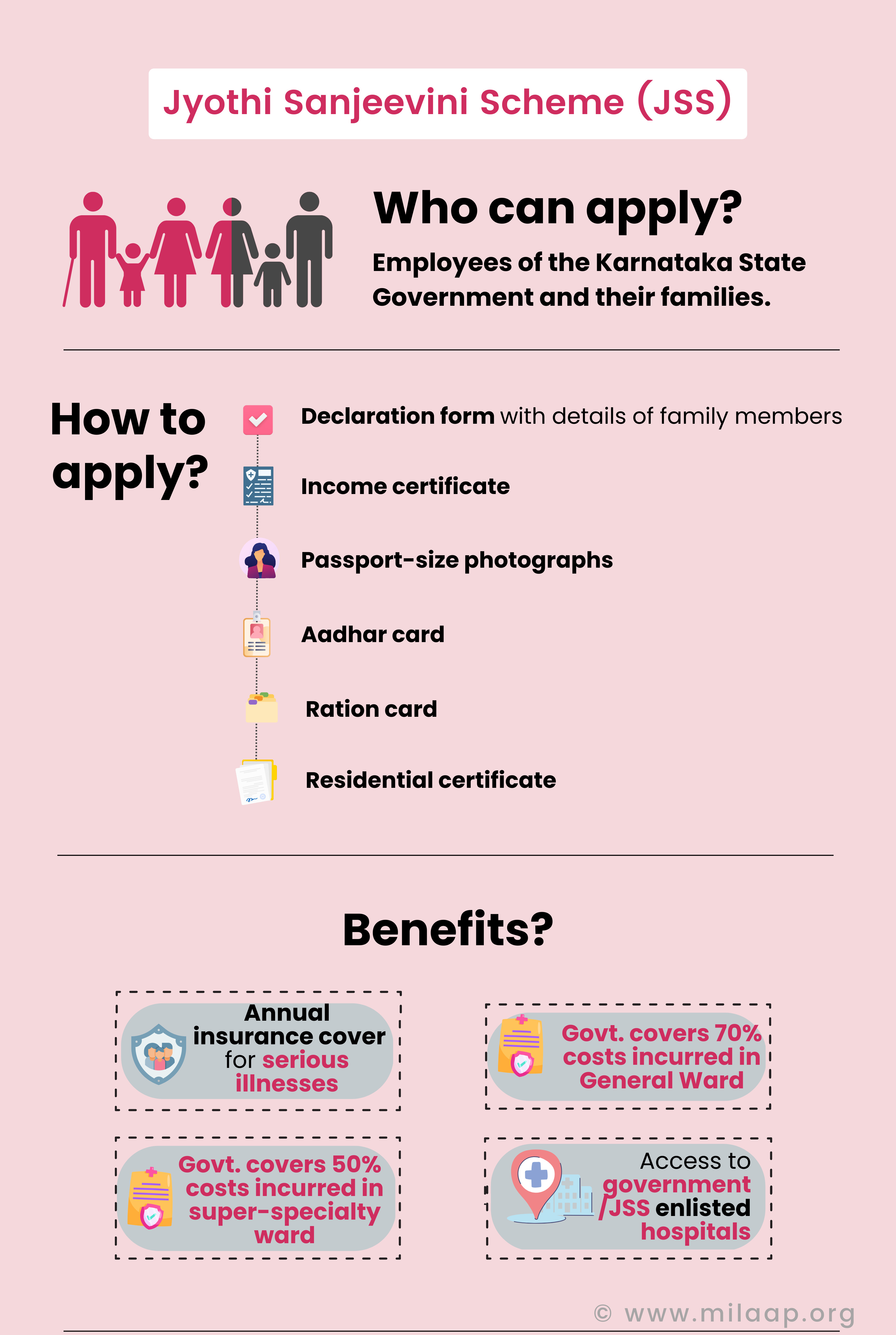
JSS is an insurance plan implemented by the Government of Karnataka that offers cashless medical aid to employees of the state government and their families, at any of the empanelled hospitals.
Read more about JSS, here.
- Any Karnataka state government employee and their family is qualified to apply for the scheme.
- The scheme provides an annual cover of ₹1.5L per year for serious illnesses requiring tertiary treatments.
- The government employee has to manage 30% of the final medical charges carried out in the general ward, while the government takes care of the remaining 70%.
- The government covers 50% of the final medical charges carried out in a super-speciality ward.
- To apply, the applicant will be required to produce a declaration form with details of the family members’ income certificate, passport-size photograph, ration card, Aadhar card, and residential certificate.
- A patient is not eligible for financial assistance under JSS if they are in any other government health insurance scheme in India.
Read more about JSS, here.
6. Health Minister’s Cancer Patients Fund (HMCPF)
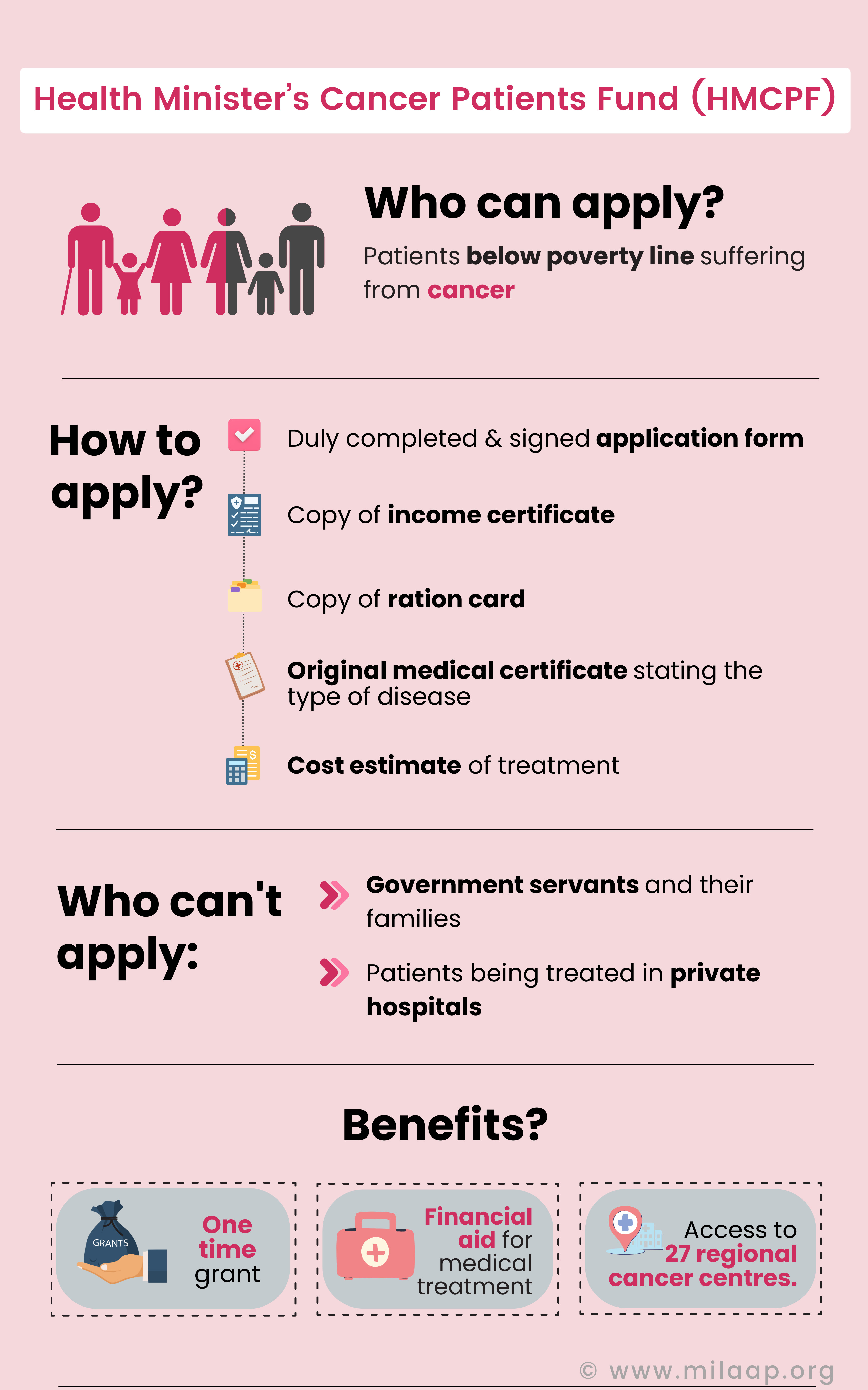
The Health Minister’s Cancer Patients Fund, a component of the umbrella scheme of Rashtriya Arogya Nidhi (RAN), provides financial assistance to patients below poverty line suffering from cancer and undergoing treatment at Karnataka's Kidwai Memorial Institute of Oncology Cancer Research and Training Centre.
Read more about HMCPF, here.
- Each cancer patient can receive a one-time grant of ₹2 lakh, up to ₹5 lakh depending on urgency.
- There is no reimbursement for expenses already incurred.
- To apply, the applicant will be required to produce a duly completed and signed application form, copy of income certificate and copy of ration card.
A patient is not eligible for financial assistance under HMCPF, if:
- Their family is covered under Pradhan Mantri Jan Arogya Yojana (PMJAY).
- They or their family member is a government servant.
- They are receiving treatment in a private hospital.
Read more about HMCPF, here.
How Milaap can help
Karnataka offers several government-sponsored schemes that provide crucial financial support for cancer patients, giving hope to those facing the high costs of treatment. However, not everyone may qualify for these schemes, and for some, the assistance provided might not be enough to cover all expenses. In such cases, Milaap can be an invaluable resource.
By creating a fundraiser on Milaap, patients and their families can bridge the financial gap, ensuring that they receive the treatment they need without delay. Milaap empowers communities to come together, offering support when government aid falls short, so no one has to face cancer alone.
By creating a fundraiser on Milaap, patients and their families can bridge the financial gap, ensuring that they receive the treatment they need without delay. Milaap empowers communities to come together, offering support when government aid falls short, so no one has to face cancer alone.







